The case for rethinking the traditional "binding-first" approach
Antibody therapeutics have revolutionised modern medicine, transforming how we treat cancer, autoimmune disorders, and infectious diseases. Yet despite the clinical success of monoclonal antibodies (mAbs), the discovery process that underpins them remains slow, inefficient, and costly. Traditional workflows continue to prioritise binding over functional relevance — often leading to the advancement of non-functional candidates and the loss of those with true therapeutic potential.

The hidden costs of binding-first workflows
Most conventional antibody discovery methods — such as hybridoma technology and single B-cell screening — focus on antibody binding. While binding is essential, it’s not a reliable predictor of therapeutic effectiveness. A binding antibody might not block a signalling pathway, trigger a desired immune response, or internalise into a cell, all of which are key mechanisms of action for therapeutic success.
Function, in contrast, provides direct evidence of biological relevance. However, in traditional workflows, functional screening is often reserved for the later stages of development and validation. By that time, substantial resources have already been spent on characterising candidates that may ultimately fail due to poor functionality.
How traditional antibody discovery fails for challenging targets
One striking example of this gap is Enlimomab, a murine anti-ICAM-1 monoclonal antibody generated using hybridoma technology. ICAM-1 is a clinically relevant target involved in inflammation and immune cell migration. But because of its low immunogenicity and high structural conservation, it presents serious discovery challenges.
Traditional methods prioritised Enlimomab’s binding properties, but failed to adequately assess its function and immunogenicity early on. The result? Enlimomab advanced to clinical trials for stroke treatment — only to worsen patient outcomes and be withdrawn. This failure highlights the risk of relying solely on binding data while overlooking function.
The limits of hybridomas and B-cell screening
Hybridoma technology, the cornerstone of antibody discovery for decades, is inherently inefficient. The fusion process can result in significant loss of antibody diversity, and there’s no equivalent fusion partner for human B-cells, requiring less efficient alternatives like Epstein-Barr virus (EBV) immortalisation.
Single B-cell screening has helped address some of these issues by enabling direct sequencing and higher-throughput candidate selection. But even with these advances, the focus remains largely on identifying antigen-binding antibodies. Functional assays are first carried out in later — and often disconnected — steps that involve different platforms, assays, and timelines.
It’s time to rethink the discovery paradigm
To accelerate timelines, reduce costs, and improve the selection of functional leads, antibody discovery must evolve beyond the binding-first mindset. A more effective approach would integrate functional screening from the outset, allowing researchers to prioritise functional candidates early in the workflow.
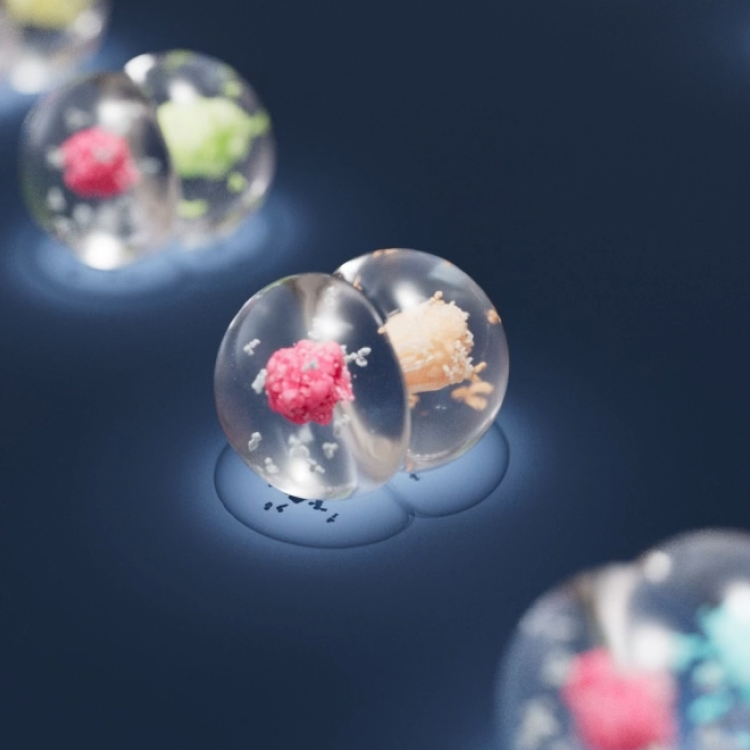
Using next-generation platforms such as Envisia enables single-cell functional screening within a unified, streamlined system. By shifting the focus from just binding to true biological effect, researchers can uncover rare, high-value leads that might otherwise be missed.
Bring function into focus
The future of antibody discovery lies not in abandoning binding assessment, but in a balanced approach. By focusing on both function and binding, we can improve lead quality, reduce attrition, and deliver better therapies faster.


.jpeg)